What’s Next: A Guide for the Potential Pfizer Authorization
Overview
Pfizer and BioNTech have submitted their application for an Emergency Use Authorization from the FDA for their COVID-19 vaccine in 5-11 year olds. The FDA is expected to grant authorization within weeks. This authorization will save lives, protect our children and bring us closer to ending this pandemic. This moment is critical for the Made to Save coalition and all organizations working on vaccine equity and access.
Many questions remain about effective outreach strategies to parents and the rollout of the authorized Pfizer vaccine for 5-11 year olds to pediatric hospitals and doctors, schools, and pharmacies. The purpose of this document is to share information that will be broadly useful to your organization as you seek to address these questions and maximize the impact of millions of children aged 5-11 becoming eligible for the COVID-19 vaccine.
Contents include:
- Timeline and process for authorization
- Parent and Caregiver Landscape, Attitudes, and Effective Talking Points
- Best Practices for Outreach to Parents and Caregivers – Our Recommendations on tactics and messages to communicate with this critical audience
Section 1: Steps and Timeline for Authorization
Below is an outline of the steps taken so far and expected timeline to EUA authorization and distribution. You can download these infographics here.
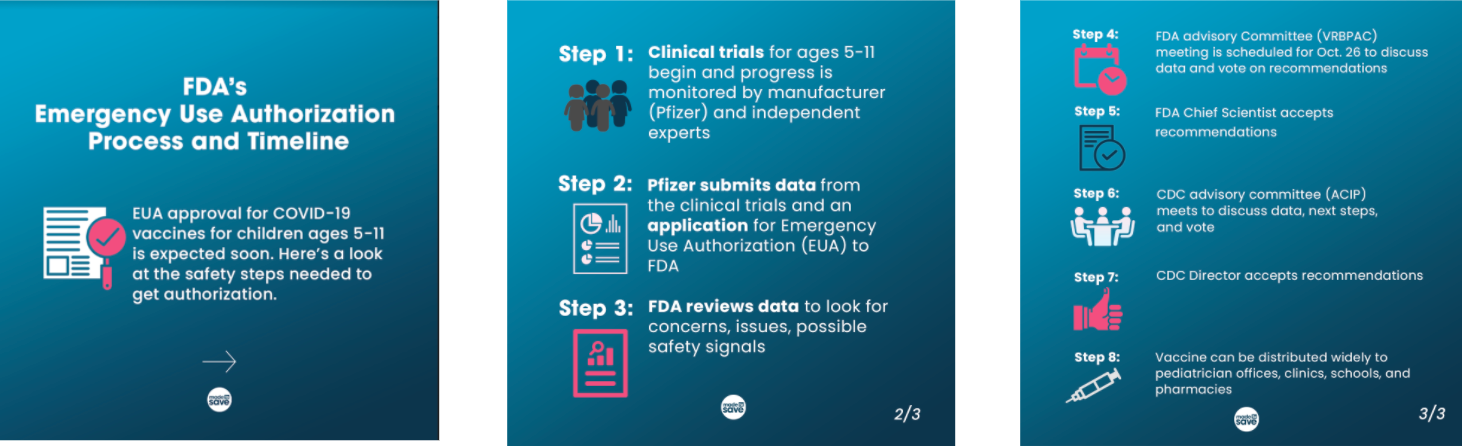
Step 1: Generally, new biologics and drugs (including vaccines and medicines) go through human trials. These trials are voluntary on the part of the participants, who are provided information, consent forms and the ability to quit the trial at any point and for any reason. The trials are overseen by Institutional Review Boards (IRB) – independent committees that review the methods proposed for research. They are also closely monitored by the drug manufacturer and an outside group of independent experts. Manufacturers like Pfizer have made a commitment to diversity in trial participants and to sharing data with the public.
Specific to Pfizer – Clinical trials in children began March 2021. In the 5-11 age group, 2,267 participants received two doses of Pfizer’s Covid-19 vaccine at ⅓ of the adult dose (10µg) given 21 days apart. Immune response was similar to participants aged 16-25 who were given the adult dose. The vaccine had similar side effects to participants aged 16-25. Pfizer has shared initial data from trials with the FDA and on 10/7 submitted the request to amend the EUA to the FDA. Additional Pfizer under 12 info.
Step 2: After trials are completed, the manufacturer submits data and a formal request for Emergency Use Authorization to the FDA. This happened on Thursday, October 7th.
Step 3: FDA staff reviews submitted data (pages and pages of individual level data) to look for concerns, issues, possible safety signals and also evaluates the effectiveness and manufacturing quality.
Step 4: The FDA’s advisory committee, VRBPAC, is scheduled to meet on October 26th, 8:30am – 5pm ET, to review the data submitted by Pfizer for amending the EUA for their Covid-19 vaccine for 5 through 11 years old. They will vote on whether they recommend EUA authorization for 5 through 11 year olds.
Step 5: FDA considers the input from the advisory committee in making a final determination to authorize the EUA. The Center for Biologics Evaluation and Research makes a recommendation and the letter of authorization is signed by the Chief Scientist.
Step 6: The CDC’s Advisory Committee on Immunization Practices (ACIP) – an independent group of medical experts – meets to discuss data, decide on details of who and when and where, and vote on recommendations.
Step 7: CDC Director considers the input from the advisory committee in making a final determination on the details of distributing the vaccines.
Step 8: Once approved or authorized by the FDA and the CDC makes recommendations for their use, vaccines can be distributed widely for use to pediatricians, primary care offices, local health departments (through local clinics, schools, vaccination sites), pharmacies, and hospitals. (NOTE: distribution methods/locations will vary widely depending on location – more information will follow when we know more.)
Section 2: Parents/Caregivers and FAQs
In this section, we include information about the landscape of parent attitudes towards vaccines for children and suggestions for messages to incorporate into your outreach.
Parent Attitudes and Landscape
About half of eligible 12-17 year olds have received at least one dose of the vaccine, with about ⅓ of parents indicating they would vaccinate their 5-11 year olds “right away” (up from 26% in July) (Kaiser Family Foundation, September 2021). Recent research has provided some insight in groups that may be more or less hesitant about vaccinating their children, which we will outline below:
Vaccinated parents have higher intentions of vaccinating their children.
Vaccinated parents are 6x more likely than unvaccinated parents to have gotten their children ages 12-17 vaccinated (de Beaumont, August 2021).
Black and Hispanic parents have more concerns about vaccinating their children than White parents.
Black and Hispanic parents are more likely to have concerns about side effects of the vaccine and future fertility than White parents. Black and Hispanic respondents are more likely to have concerns about their individual accessibility to the vaccine (e.g., time off work, traveling to get vaccine, out of pocket cost, trustworthiness of vaccination site) (Kaiser Family Foundation, August 2021).
Catholic parents are more likely to vaccinate their children, particularly if they are people of color.
A poll by the Public Religion Research Interest Group reported Catholic parents had the most positive attitudes towards vaccination than other religious groups surveyed with 48% of Hispanic Catholics and 40% of White Catholics reporting they have gotten or will get their children vaccinated. The lowest levels of intentions were from Evangelical Protestants (27% of Hispanic Protestants, 18% of White Evangelicals) (National Catholic Reporter, August 2021).
Getting parents on the same page about vaccinating their children is key.
Mothers may be more skeptical of vaccines than fathers: 27% of mothers say they are extremely unlikely to vaccinate their children versus 14% of fathers (COVID States Project, March 2021, Pre-Print available). Children of divorced parents with contrasting COVID-19 vaccine beliefs are less likely to get vaccinated (Web MD, July 2021).
Acknowledge the decision to vaccinate children is both a parenting decision and a health decision.
A focus group study (conducted in both English and Spanish) revealed that effective messaging involves framing the vaccination decision as both a parenting decision and a health decision: rather than leading with data points, build trust and affinity with messengers who are also parents, acknowledge and affirm parents’ concerns with the decision, and allow parents to ask questions to feel confident about their decision (Goodwin Simon Strategic Research, July 2021).
Messaging to Parents of Color
Based on the research and information above, here are the best messages we recommend incorporating into your outreach to parents, caregivers, and guardians of color:
1. Vaccinating children against COVID-19 can help protect them from dangerous variants, hospitalization, or developing long-term COVID-19 symptoms.
2. If children are vaccinated against COVID-19, they can focus on their learning and reap the rewards of in-person learning experience.
3. Long-standing scientific evidence shows that other vaccines protect children against dangerous viruses and diseases, just as the COVID-19 vaccines do.
4. Vaccinating children against COVD-19 can in turn help protect the people around them who are at high risk of having severe effects from COVID-19, whether family members, classmates, teachers, or people in their communities.
5. The Pfizer emergency use authorization for 5- to 11- year-olds is an important milestone in the COVID-19 pandemic, one that will enable us to protect a larger segment of our population.
de Beaumont and Made to Save also developed guidance in August 2021 for communicating to parents about vaccines and COVID-19 in schools.
Frequently Asked Questions (FAQs)
Q1: Approximately how many children (0-18 years old) in the United States have gotten COVID-19?
According to the CDC COVID Data Tracker (as of Oct. 7), children ages 5-11 account for over a million cases (5% of all COVID-19 cases) and 136 deaths. Since the pandemic began, children represented 16.0% of total cases. That percentage is increasing as more adults get vaccinated. For the week ending September 30, children were 27% of reported weekly COVID-19 cases (children, under age 18, make up 22% of the US population).1
Q2: What are the long term effects of the vaccine on children? How can we be sure that the vaccine is safe?
Just as with other vaccines, this vaccine is expected to have short-term side effects like a sore arm and fever. The anti-vaccine industry has spread rumors of long-term impacts including on fertility, but the vaccine is gone from your system within days. In the history of vaccines, reactions typically show up within a few weeks after the shot. We have not seen long-term side effects after nearly a year of giving the vaccine to hundreds of millions of adults, and we do not expect to see long-term effects in kids besides being protected against COVID-19. Additionally, medical researchers are constantly monitoring to make sure they catch and can tell the public about even very rare side effects.
Q3: Will the COVID-19 vaccine affect my child’s fertility?
No. There is no evidence that fertility problems are a side effect of any vaccine, including COVID-19 vaccines.2 The American College of Obstetrics and Gynecology and the American Society for Reproductive Medicine (fertility specialists) both strongly recommend that people get the COVID-19 vaccine.3
Q4: How do I get my child vaccinated?
The vaccine will be available at many pediatrician and family practice clinics, local health departments, community health centers, pharmacies, school-based health centers, and other places where kids usually go for their vaccines. Some schools may also have vaccines available for families. Check with your usual medical provider or local health department4 when vaccines are authorized to see where you can go.
Q5: Why should I get my child vaccinated if children are less likely to experience severe or life-threatening effects of COVID-19?
Getting your child vaccinated can prevent them from getting and spreading the virus to more vulnerable family and community members. If your child gets COVID-19, the vaccine can also help prevent them from becoming severely-ill or protect them from having any long-term side effects.
Q6: Do I need to be present when my child is vaccinated?
States differ in their consent requirements for minors. Many require parental consent, with some additionally requiring a parent or adult to be present. A database of state parental consent laws has been compiled by Kaiser Family Foundation.
Q7: Can my kid get the COVID-19 vaccine at the same time as other shots?
According to the CDC, routine childhood immunizations and flu shots can be safely co-administered.
Section 3: Outreach Best Practices
Parents are a unique audience for vaccine information. In addition to answering their questions about how and where to get their children vaccinated, we must also address their specific concerns about the vaccine in children 5-11. Below we’ve compiled some initial learning on effective outreach to parents.
Tips from our grantees and partners
— Provide in-language + visual messaging: Reach the most parents by providing information and education in multiple languages, as well as providing visual messaging that can be easily understood in lower literacy populations.
— Include parent messaging in pre-existing outreach efforts: If you are already having conversations about the vaccines (at events, through canvassing, via text, etc.), this is a great time to include messaging for parents to find out if they have questions about the vaccines for 5-11 year olds. Here are some sample scripts you can use or incorporate into your own.
— Identify trusted messengers for parents:
– Schools have historically served as vaccination sites and health hubs for children and can still be a resource for providing pediatric care and information.
– The Oregon Department of Public Health developed a series of videos based on focus group research that featured pediatricians who were also parents. Seeing doctors who are also parents helps build credibility and trustworthiness (Goodwin Simon Strategic Research, July 2021).
— Provide information and conversations to parents through high traffic canvassing: By targeting locations where there are likely to be parents, you will be able to more easily engage this demographic in conversations about childhood vaccines. Some possible locations include school drop-offs and pickups, health clinics, social service centers, community colleges, and retailers such as Walmart, Target, etc.
Using the TEO method with parents and caregivers
Made to Save uses an active listening model, called the TEO method, to encourage trusted messengers to have COVID-19 vaccine conversations with their friends and family members. You can replicate this model when having a conversation with a parent or caregiver that has questions and concerns about vaccinating their children.
These conversations are meant to support someone into making a decision to get vaccinated, but it is not our job to tell them what to do or how they should feel. It may also take multiple conversations before someone makes a decision to get their children vaccinated.
Build Trust and Understand
Listen to understand, not to respond. Don’t form your reply before the person is done speaking. Invite them to share until you feel you understand what’s holding them back.
Ask questions to get to the root of the concern. “So you’re nervous about the side effects your children may experience? [Pause to listen and prompt the person if needed:] Tell me more.”
Repeat back or state a summary. “Thank you for sharing that with me. What I am hearing you say is [INSERT SUMMARY STATEMENT]….”
Listen for: what, if anything is holding them back? If they just need help with access, offer to help! Give them information, make an appointment for them, find them a ride – whatever you can do to help! If they have concerns about the vaccine itself, respond authentically and plan to follow up.
Demonstrate Empathy
Express empathy and connect on values. Acknowledge and relate to what the person is sharing. Validating concerns, expressing empathy, and demonstrating that you understand will help make the person feel more comfortable. “I see that you feel nervous about making such an important decision about your children’s health, that makes sense that you feel that way.”
Respond without judgement and avoid making assumptions. “I see where you’re coming from. It can be hard to know what information on social media is real when there is so much misinformation and clickbait.”
Help them find their own reason for vaccination
Ask for permission to share: “You know, I’ve heard that concern before and I’ve looked into it. Would you mind if I shared with you what I found out?”
Pair shared values with key facts. “I hear that protecting your children is very important to you. The data that the FDA is showing shows that the vaccine is really good at protecting children.”
Help them find their own reason for vaccination: The reasons that someone may choose to get vaccinated will always be those that are most compelling to them personally. “I am getting my children vaccinated so that they can attend summer camp next year. What benefits could you see in vaccinating your children?”
Don’t tell them what to do or think. It is important to guide a person to make their own decision rather than the lecture or dictate what someone should do or think.
Texting
Over the course of Sept 23rd – Sept 27th, Made to Save sent 20,000 texts to likely parents under the age of 50 asking if they were planning on getting their 5-11 year old children vaccinated once the FDA approved Emergency Use Authorization (EUA) for the Pfizer vaccine. Half were sent to parents who were likely to be vaccinated, while the other half were sent to parents unlikely to be vaccinated.
In the vaccinated-parent group, we saw that only 77% of respondents were planning on getting their children vaccinated. One-fifth (20%) said they were not planning on getting their child vaccinated. This group also had a contact rate of 17.8%, double the usual peer-to-peer SMS average.
Key takeaway: Texting vaccinated people can lead to much higher contact rates than normal peer to peer SMS campaigns, and organizations that employ relational programs should consider ways to contact vaccinated people to increase vaccine uptake amongst unvaccinated people. Even among the vaccinated-parent group, there were still 20% of parents who were unsure about getting their children vaccinated, which makes a great opportunity for high-contact rate persuasion targets.
Additional Resources
- Vaccine Equity Cooperative: Planning for the Child (5-11) Vaccine Rollout
- CDC COVID Data Tracker (Oct. 7, 2021):
-
- For ages 5-11, there have been over a million cases (5% of all COVID cases) and 136 deaths (less than < .01%)
- This resource breaks down youth cases by vaccine authorization group (e.g., 5-11, 12-17)
- Hospitalizations have increased for those under 18, particularly around September.
- American Academy of Pediatrics (Last Updated: Sept. 30, 2021):
- Data based on state data (those reporting — 49 plus DC) though age breakdown of “child” varied by state“, summarized weekly. The latest report is September 30..
- Hospitalization rates vary by state, with children ranging from approximately 2-4% of their total accumulated hospitalizations and up to 2% of all their child COVID-19 cases resulting in hospitalization.
- Case rates peaked around the beginning of September (likely around when schools were opening), and that varied by region (more cases in South).
1. Source: American Academy of Pediatrics (Last Updated: Sept. 30, 2021)
2. Source: American Academy of Family Physicians
3. Source: ACOG
4. Source: CDC
